Did you know that glaucoma is one of the leading causes of irreversible blindness worldwide? The worrying aspect is that this disease often progresses silently, with no clear symptoms in its early stages, leaving many patients unaware that they are gradually losing their vision until the condition becomes severe. Recognizing and detecting early signs of glaucoma is the golden key to saving your sight.
This article is a comprehensive guide to understanding glaucoma: from its definition, the importance of early detection, the early signs of glaucoma you shouldn’t ignore, to risk factors, diagnostic methods, treatment options, and how to live with the condition. The goal is to equip you with the necessary knowledge to proactively protect your eyes and preserve your precious vision.
What is Glaucoma?
Glaucoma is a group of eye conditions that cause damage to the optic nerve – the essential nerve that transmits visual information from the eye to the brain. This damage is often directly related to increased pressure inside the eye (intraocular pressure – IOP). However, it’s important to remember that glaucoma can still occur even with normal IOP levels.
Normally, our eyes continuously produce a clear fluid called aqueous humor to nourish the internal structures. This fluid also continuously drains out of the eye through a drainage system. When there is an imbalance between the production and drainage of aqueous humor, IOP increases, leading to gradual compression and damage to the optic nerve fibers. Once the optic nerve is damaged, it cannot recover, resulting in permanent vision loss starting from the periphery (side vision) and gradually narrowing towards the center, eventually leading to complete blindness.
There are two main types of glaucoma:
- Primary Open-Angle Glaucoma (POAG): This is the most common type, accounting for about 90% of cases. It usually progresses very subtly, with no clear symptoms in the early stages. The eye’s drainage system slowly becomes clogged over time, causing IOP to gradually increase without pain.
- Acute Angle-Closure Glaucoma (AACG): This type is less common but more dangerous. It occurs when the drainage angle is suddenly blocked, causing a rapid and sudden increase in IOP. Symptoms are usually severe, such as intense eye pain, redness, blurred vision, halos around lights, nausea, and vomiting. This is a medical emergency that requires immediate treatment to prevent permanent vision loss within hours or days.
Additionally, there are secondary glaucoma (due to other conditions like eye injury, inflammation, prolonged medication use) and congenital glaucoma (rare in young children).
Why is Early Detection of Glaucoma So Important?
The importance of early detection of glaucoma cannot be overstated, for the following reasons:
- Irreversible damage: Optic nerve damage caused by glaucoma is permanent and irreversible. Once vision is lost due to this disease, it cannot be restored by any treatment method.
- Silent progression: Especially with open-angle glaucoma, the disease often causes no pain or any noticeable early signs until significant damage has occurred and a portion of the visual field is lost. By the time patients start noticing vision problems (e.g., loss of peripheral vision), the disease is usually in an advanced stage.
- Stopping progression: The main goal of glaucoma treatment is to control IOP to prevent or slow down further optic nerve damage, thereby preserving remaining vision. The earlier it’s detected, the sooner a doctor can start treatment, helping to better protect vision.
- Saving vision: Early detection allows doctors to apply effective treatments (eye drops, laser, surgery) to lower IOP, prevent further damage, and preserve existing vision. This helps patients maintain their quality of life and independence in daily activities.
- Preventing blindness: Without timely diagnosis and treatment, glaucoma will inevitably lead to complete blindness. Regular eye exams, especially for those with risk factors, are the only way to detect glaucoma early and avoid this unfortunate outcome.
>> Common Retinal Diseases and Effective Prevention Methods
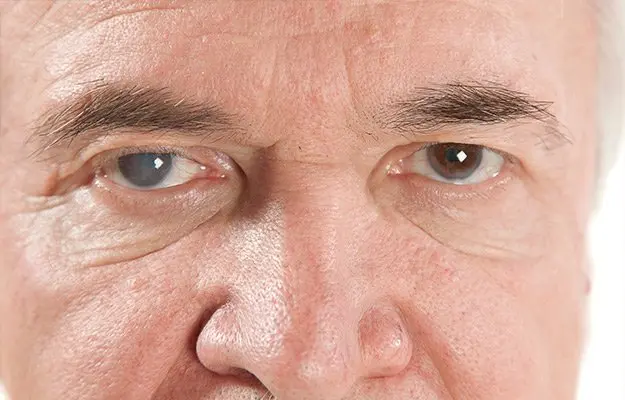
Early Signs of Glaucoma
As mentioned, early signs of glaucoma (especially the open-angle type) are often difficult to recognize. However, if you pay attention, you might notice some subtle changes or transient symptoms. Being aware of these signs of glaucoma is extremely important:
- Gradual loss of peripheral vision (side vision): This is the most classic sign of open-angle glaucoma, but it’s often only noticed when the disease has progressed. Initially, you might bump into objects on the sides, or have difficulty seeing objects outside your direct line of sight. This usually happens very slowly and goes unnoticed until significant damage.
- Seeing halos or rainbows around lights: Especially at night or in low light conditions, you might see colored circles or halos around light sources (streetlights, car headlights). This is a sign of mild corneal swelling due to increased IOP.
- Mild eye pain or unexplained discomfort: Although open-angle glaucoma usually doesn’t cause pain, you might sometimes feel slight pressure, tightness, or a dull ache in your eyes.
- Temporary blurred vision or unstable vision changes: Vision might become temporarily blurry, especially in the morning or after waking up. Or you might feel the need to change your glasses more frequently without significant improvement in vision.
- Mild headache in the forehead or temple area: Increased IOP can put pressure on the nerves around the eyes, leading to mild headaches, often concentrated in the forehead or temple region, sometimes radiating to the back of the head.
- Nausea or vomiting (especially in acute cases): This is a serious symptom of acute angle-closure glaucoma. Accompanied by severe eye pain, eye redness, sudden blurred vision, nausea, or vomiting, it’s an urgent sign requiring immediate medical attention.
- Unexplained eye redness: In cases of acute angle-closure glaucoma, the eye can appear bright red due to increased pressure on blood vessels.
Importantly, many early signs of glaucoma are vague and can be confused with other conditions. Therefore, the best way to detect glaucoma early is through regular eye exams with an ophthalmologist, especially if you have risk factors.
When to See an Ophthalmologist for Glaucoma Screening?
Regular eye exams are the only way to detect glaucoma early, especially the open-angle type. You should proactively seek an ophthalmologist in the following cases:
- Routine eye exams:
- People under 40 with no risk factors: Every 2-4 years.
- People aged 40-54: Every 1-3 years.
- People aged 55-64: Every 1-2 years.
- People aged 65 and older: Every 6-12 months.
- When you have high risk factors: If you belong to a high-risk group (listed in the next section), you should start regular eye exams earlier and more frequently as recommended by your doctor, regardless of age.
- When any suspicious signs appear: If you notice any of the early signs of glaucoma mentioned above (temporary blurred vision, seeing halos, mild unexplained headache, feeling of eye pressure), even if fleeting, schedule an appointment with an ophthalmologist.
- Emergency (suspected acute angle-closure glaucoma): You need to go to an emergency room or eye hospital immediately if you suddenly experience the following symptoms:
- Sudden, severe eye pain.
- Severe headache.
- Severe blurred vision or sudden vision loss.
- Very clear halos around lights.
- Nausea or vomiting.
- Severe eye redness.
These symptoms may indicate an acute glaucoma attack, which, if not treated promptly within hours, can lead to permanent blindness.
Glaucoma Risk Factors
While anyone can develop glaucoma, some groups of people are significantly more at risk. If you belong to these groups, regular eye exams become even more important:
- Age: The risk of developing glaucoma increases significantly after age 40 and continues to rise with age. People over 60 have the highest risk.
- Family history: If you have a close relative (parent, sibling) with glaucoma, your risk is 4-9 times higher than that of the general population. Genetics play a significant role.
- Ethnicity: People of African and Hispanic descent have a higher risk of open-angle glaucoma and it often starts earlier and progresses more severely. People of Asian descent have a higher risk of angle-closure glaucoma.
- Diabetes: Diabetes, especially poorly controlled diabetes, increases the risk of glaucoma.
- Severe high or low blood pressure: Both excessively high and low blood pressure can affect blood flow to the optic nerve.
- Cardiovascular disease: Conditions affecting blood circulation can cause optic nerve damage.
- High myopia (nearsightedness): People with severe nearsightedness (high refractive error) have eye structures that are more susceptible to optic nerve damage.
- Prolonged corticosteroid use: Especially long-term use of corticosteroid eye drops or oral corticosteroids can significantly increase IOP.
- Previous eye injury: Severe eye trauma can damage the eye’s drainage system, leading to glaucoma many years later.
- Certain other eye conditions: For example, uveitis, retinal detachment.
If you have one or more of the risk factors above, do not wait until you notice early signs of glaucoma to get examined. Proactively discuss with your ophthalmologist about the appropriate frequency of eye exams for yourself.
>> Read more: Ocular Albinism: Causes, Symptoms, and Effective Treatment Options
Glaucoma Diagnostic Methods
To diagnose glaucoma and assess the extent of damage, an ophthalmologist will perform a series of specialized tests, not just simply measuring IOP. These tests include:
- Tonometry: This is the basic and most important test, used to measure the pressure inside the eye. There are various methods of tonometry.
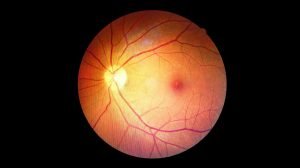
- Fundus examination and optic nerve assessment: The doctor will use a specialized microscope to directly observe the optic nerve at the back of the eye. They will look for characteristic signs of glaucoma damage, such as greater-than-normal optic disc cupping or color changes.
- Visual Field Test: This test evaluates your peripheral vision to see if there are any blind spots caused by optic nerve damage. You will look at a screen and press a button when a light appears at different locations.
- Optical Coherence Tomography (OCT): This is an advanced imaging technique that creates detailed cross-sectional images of the retina and optic nerve. OCT can detect very small changes in the retinal nerve fiber layer, helping with early diagnosis and monitoring disease progression before it shows up on visual field tests.
- Gonioscopy: The doctor will use a special contact lens to examine the eye’s drainage angle, determining whether it is open or closed.
- Central Corneal Thickness (Pachymetry): Corneal thickness can affect IOP readings. A thin cornea can result in a lower-than-actual measured IOP, and vice versa.
All these tests together help the doctor make an accurate diagnosis of the type of glaucoma, its severity, and determine the appropriate glaucoma treatment plan.
Glaucoma Treatment
The main goal of glaucoma treatment is to lower intraocular pressure to a safe level to prevent or slow down further optic nerve damage, thereby preserving remaining vision. As mentioned, optic nerve damage is permanent, so treatment cannot restore lost vision but only prevent further damage.
The main glaucoma treatment methods include:
- Eye drops: This is the first and most common treatment option for most types of glaucoma. Eye drops work by reducing the production of aqueous humor or increasing its drainage from the eye.
- Examples: Prostaglandin analogs (latanoprost, travoprost), Beta-blockers (timolol), Alpha-agonists (brimonidine), Carbonic anhydrase inhibitors (dorzolamide).
- Eye drop use must strictly adhere to the doctor’s instructions regarding dosage and frequency, even if there are no symptoms.
- Laser treatment:
- Selective Laser Trabeculoplasty (SLT) / Argon Laser Trabeculoplasty (ALT): Uses laser to improve the eye’s drainage system, helping aqueous humor drain more easily and reduce IOP. Often used for open-angle glaucoma.
- Laser Iridotomy: Creates a small hole in the iris to relieve pressure in the eye, usually applied for angle-closure glaucoma.
- Laser treatment can be effective for a period but is not a permanent solution and may need to be repeated or combined with medication.
- Surgery (Glaucoma Surgery): Surgery is considered when eye drops and laser treatment are not sufficient to control IOP, or when the disease has progressed severely.
- Trabeculectomy: Creates a new drainage channel in the eye to allow aqueous humor to flow out, helping to reduce IOP.
- Glaucoma Drainage Devices: A small device is implanted in the eye to drain aqueous humor.
- Minimally Invasive Glaucoma Surgery (MIGS): These are newer, less invasive surgical techniques, often combined with cataract surgery to lower IOP.
- Surgery is generally highly effective in reducing IOP, but also carries certain risks and requires a recovery period.
Important note: Patients with glaucoma require lifelong monitoring. Treatment is an ongoing process, not a complete cure. Adherence to treatment, regular follow-up appointments, and close cooperation with your doctor are decisive factors in preserving vision.
Living with Glaucoma: Advice and Care
Living with glaucoma requires patience, discipline, and some lifestyle changes. Here are some helpful tips to better manage the condition and maintain your quality of life:
- Strictly follow your treatment plan: This is the most important thing. Use eye drops at the correct time and dosage as instructed by your doctor. Do not arbitrarily stop medication or change the dosage even if your eyes feel better.
- Regular follow-up appointments: The follow-up schedule prescribed by your ophthalmologist is crucial for monitoring IOP, evaluating the condition of the optic nerve and visual field, and adjusting the treatment method when needed.
- Report any changes and side effects: If you experience any side effects from eye drops (dry eyes, redness, itching, blurred vision) or new symptoms, report them immediately to your doctor for advice and adjustment.
- Healthy diet:
- Eat plenty of dark green vegetables, fruits rich in vitamins A, C, E, and antioxidants.
- Limit processed foods, sugary drinks, and saturated fats.
- Avoid drinking too much water at once (more than 1 liter) as it can temporarily increase IOP.
- Regular exercise: Moderate exercise such as brisk walking, jogging, and swimming can help lower IOP in some people. However, avoid exercises that cause straining or holding your breath for too long.
- Reduce stress: Stress can affect IOP and overall health. Find ways to relax such as meditation, yoga, listening to music, or reading.
- Proper sleeping posture: Elevating the head of your bed by about 20 degrees when sleeping can help reduce IOP while asleep.
- Avoid medications that increase IOP: Some medications (e.g., antihistamines, tricyclic antidepressants, asthma medications containing corticosteroids) can increase IOP. Always inform your doctor about all medications you are currently taking.
- Wear protective eyewear: Protect your eyes from injury when participating in sports or working in hazardous environments.
- Quit smoking and limit alcohol: Smoking and excessive alcohol consumption can negatively affect eye and overall health.
- Seek support: Connect with glaucoma patient support groups or share with family and friends for encouragement and advice.
Living with glaucoma is a long journey, but with proper care and treatment adherence, you can fully control the disease and maintain your vision and quality of life as best as possible.
Conclusion
Glaucoma is a silent enemy of vision. It can steal your sight without warning, especially in its early stages. However, with the right knowledge and proactive measures, you can fully control and protect your eyes.
Recognizing the early signs of glaucoma, understanding the risk factors, and most importantly, undergoing regular eye exams are the best shields against the disease. Don’t wait until your vision is affected; proactively see an ophthalmologist today to check your eye health.
Remember, vision lost due to glaucoma cannot be regained, but you can absolutely preserve your remaining vision by detecting and treating it promptly. Your eyes are the windows to your soul; take the best care of them!