Diabetic Retinopathy: Symptoms, Stages, Causes and Treatments
What is diabetic retinopathy?
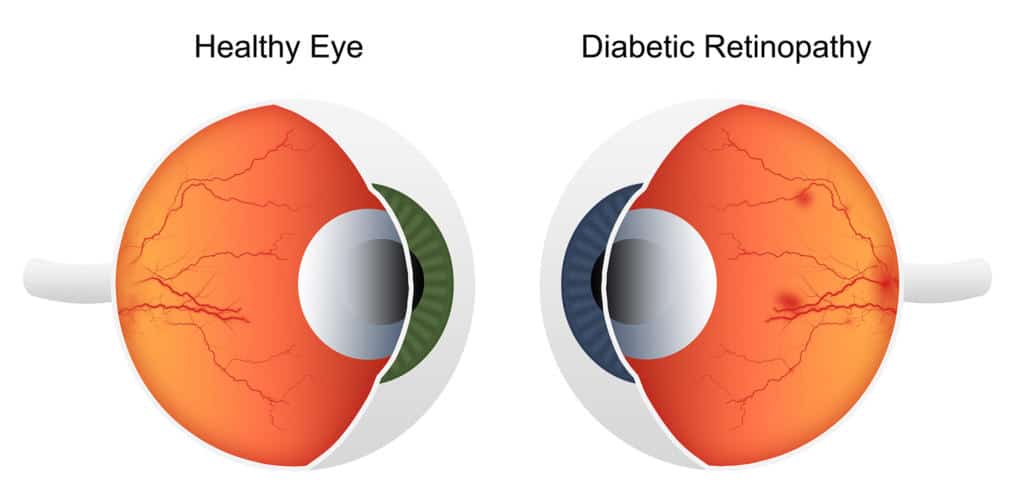
Diabetic retinopathy is a serious eye condition that can develop in people with diabetes. It occurs when high blood sugar levels over time cause damage to the blood vessels in the retina, which is the light-sensitive tissue located at the back of the eye. The retina is responsible for capturing visual images and transmitting them to the brain through the optic nerve.
When the blood vessels in the retina are damaged, they may leak blood or fluid, leading to swelling and distortion of the retinal tissue. In response to this damage, the body may attempt to grow new, fragile blood vessels to compensate for the impaired blood flow. However, these new blood vessels are often weak and prone to leakage, causing further damage to the retina and potentially leading to severe vision problems.
Diabetic retinopathy symptoms
In the early stages of diabetic retinopathy, there may be little to no noticeable symptoms. As the condition progresses, symptoms may become more apparent. The symptoms of diabetic retinopathy can affect one or both eyes and may include:
- Blurred Vision: Blurred vision is a common symptom of diabetic retinopathy. The blurriness can affect both near and distance vision and may vary in intensity.
- Floaters: Floaters are small, dark spots or lines that appear to float in the field of vision. They are caused by tiny specks of blood or other fluids in the vitreous humor of the eye.
- Fluctuating Vision: Vision may fluctuate or change throughout the day, especially if diabetic macular edema (DME) is present. DME is the accumulation of fluid in the macula, the central part of the retina.
- Impaired Color Vision: Colors may appear faded or less vibrant than usual.
- Dark or Empty Areas in Vision: Some people may experience blind spots or areas of reduced vision.
- Difficulty Reading or Seeing Fine Details: Reading or performing tasks that require clear vision may become challenging.
- Vision Loss: In severe cases, diabetic retinopathy can lead to significant vision loss or even blindness.
Diabetic retinopathy stages
Diabetic retinopathy progresses through several stages, each characterized by specific changes in the blood vessels of the retina. The stages of diabetic retinopathy are as follows:
Stage 1: Mild Non-Proliferative Diabetic Retinopathy (NPDR)
- At this early stage, small areas of the blood vessels in the retina may weaken and become dilated. These areas are called microaneurysms.
- Some blood vessels may leak fluid or blood into the retina, leading to the formation of small retinal hemorrhages or tiny dot-like spots of blood in the retina.
- There may be mild swelling or edema in the retina, which is referred to as macular edema. The macula is the central part of the retina responsible for detailed vision, and its involvement can cause central vision blurriness.
Stage 2: Moderate Non-Proliferative Diabetic Retinopathy (NPDR)
- In this stage, the number of microaneurysms and retinal hemorrhages increases.
- The blood vessel abnormalities may cause the retina to become ischemic, meaning that some areas are deprived of oxygen due to impaired blood flow.
Stage 3: Severe Non-Proliferative Diabetic Retinopathy (NPDR)
- In severe NPDR, a more significant number of blood vessels become blocked, leading to widespread retinal ischemia.
- The lack of oxygen triggers the release of growth factors, which promote the development of abnormal blood vessels (neovascularization) in the retina.
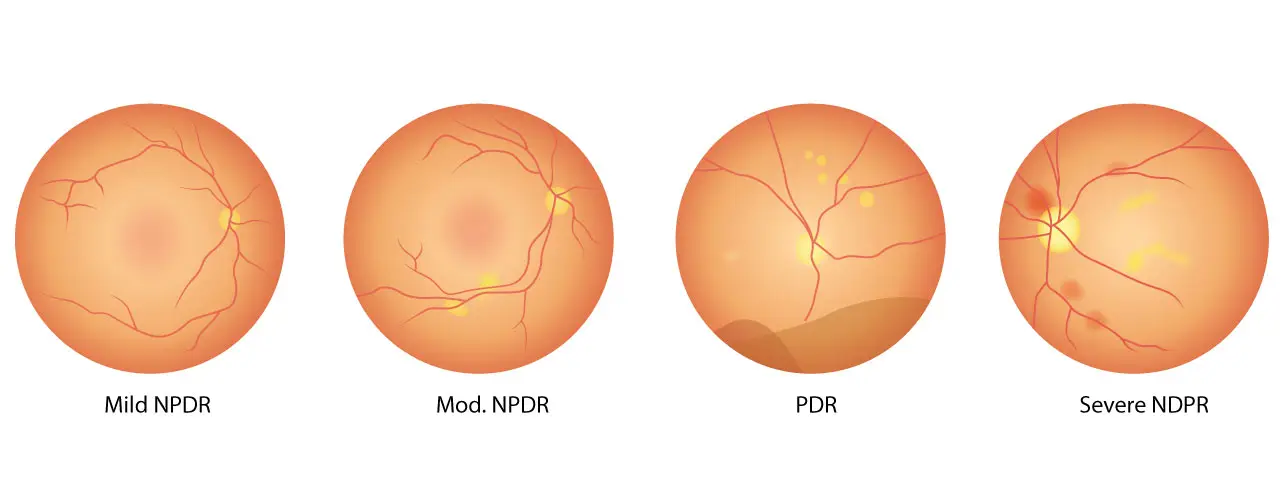
Stage 4: Proliferative Diabetic Retinopathy (PDR)
- PDR is the advanced stage of diabetic retinopathy characterized by the presence of new, abnormal blood vessels (neovascularization).
- These fragile blood vessels can leak blood into the vitreous humor, causing floaters and potentially leading to vitreous hemorrhage (bleeding into the eye’s gel-like substance).
- In some cases, the new blood vessels may contract and pull on the retina, leading to retinal detachment. This can cause severe vision loss or blindness if not treated promptly.
Causes of diabetic retinopathy
Diabetic retinopathy is primarily caused by the long-term effects of diabetes, particularly when blood sugar levels are poorly controlled. The main causes of diabetic retinopathy include:
- High Blood Sugar Levels (Hyperglycemia): Prolonged periods of elevated blood sugar levels in people with diabetes can damage the blood vessels in the retina.
- Duration of Diabetes: The longer a person has diabetes, the higher the risk of developing diabetic retinopathy.
- Type of Diabetes: Both type 1 and type 2 diabetes can lead to diabetic retinopathy.
- Blood Pressure: Uncontrolled hypertension (high blood pressure) can exacerbate the effects of diabetic retinopathy.
- Cholesterol Levels: Elevated levels of cholesterol and triglycerides in the blood can contribute to the progression of diabetic retinopathy.
- Pregnancy: Pregnant women with diabetes, particularly those with poorly controlled blood sugar levels during pregnancy (gestational diabetes), may be at higher risk of developing or worsening diabetic retinopathy due to hormonal changes and shifts in blood sugar levels.
- Smoking: Smoking can damage blood vessels throughout the body, including those in the retina, and can accelerate the progression of the disease.
Diabetic retinopathy treatment
Laser Photocoagulation (Laser Treatment):
- Description: Laser photocoagulation is a non-invasive procedure that uses a focused laser beam to treat diabetic retinopathy. The laser creates small, controlled burns on the retina, causing coagulation and sealing off leaking blood vessels. It also helps to reduce the growth of abnormal blood vessels.
- Indications: Laser photocoagulation is effective in managing both non-proliferative diabetic retinopathy (NPDR) and proliferative diabetic retinopathy (PDR). For NPDR, it helps to control macular edema and reduce swelling in the retina. In PDR, the laser treatment aims to prevent the growth of fragile and abnormal blood vessels, which can lead to retinal bleeding and detachment.
- Procedure: Laser photocoagulation is typically performed in an outpatient setting. The ophthalmologist dilates the patient’s pupils using eye drops and applies numbing drops to make the procedure more comfortable. The patient sits facing a specialized microscope, and the ophthalmologist directs the laser to target specific areas of the retina. The procedure can take about 15 to 30 minutes, and patients can usually return home the same day.
Intravitreal Injections (Anti-VEGF Therapy):
- Description: Intravitreal injections involve the direct delivery of medication into the vitreous humor of the eye. Anti-VEGF medications are used to block the action of Vascular Endothelial Growth Factor (VEGF), a protein that promotes the growth of abnormal blood vessels and increases vascular permeability in the retina.
- Indications: Intravitreal injections are particularly effective in managing diabetic macular edema (DME) and some cases of proliferative diabetic retinopathy (PDR). By reducing fluid leakage and swelling in the retina, these injections can improve vision and slow down the progression of the disease.
- Procedure: The intravitreal injection is performed in the ophthalmologist’s office or a specialized clinic. Before the injection, the eye is numbed with local anesthesia to minimize discomfort. Using a thin needle, the anti-VEGF medication is precisely injected into the vitreous humor. After the procedure, patients may be advised to rest for a short period before being allowed to go home.
Vitrectomy:
- Description: Vitrectomy is a surgical procedure used in advanced cases of diabetic retinopathy, especially when there is significant bleeding (vitreous hemorrhage) or retinal detachment. It involves removing the vitreous gel that fills the center of the eye, along with any blood or scar tissue that may be present. This procedure helps to clear the visual field and improve vision.
- Indications: Vitrectomy is typically considered when other treatments, such as laser photocoagulation and intravitreal injections, have not been successful in managing the complications of diabetic retinopathy. It is reserved for severe cases with vitreous hemorrhage or retinal detachment.
- Procedure: Vitrectomy is performed in an operating room under local or general anesthesia, depending on the patient’s condition and surgeon’s preference. Microsurgical instruments are used to make small incisions in the eye, through which the vitreous gel is removed. The vitreous cavity is then filled with a clear saline solution. The procedure may take a few hours, and patients may need to stay in the hospital for a short observation period before being discharged.

Diabetic retinopathy ICD-10
In the International Classification of Diseases, Tenth Revision (ICD-10), the code for diabetic retinopathy is as follows:
E11.3 – Type 2 diabetes mellitus with ophthalmic complications
- E11.32 – Type 2 diabetes mellitus with mild nonproliferative diabetic retinopathy
- E11.33 – Type 2 diabetes mellitus with moderate nonproliferative diabetic retinopathy
- E11.34 – Type 2 diabetes mellitus with severe nonproliferative diabetic retinopathy
- E11.35 – Type 2 diabetes mellitus with proliferative diabetic retinopathy
- E11.36 – Type 2 diabetes mellitus with diabetic cataract
- E11.37 – Type 2 diabetes mellitus with diabetic macular edema
- E11.39 – Type 2 diabetes mellitus with other diabetic ophthalmic complication
E10.3 – Type 1 diabetes mellitus with ophthalmic complications
- E10.32 – Type 1 diabetes mellitus with mild nonproliferative diabetic retinopathy
- E10.33 – Type 1 diabetes mellitus with moderate nonproliferative diabetic retinopathy
- E10.34 – Type 1 diabetes mellitus with severe nonproliferative diabetic retinopathy
- E10.35 – Type 1 diabetes mellitus with proliferative diabetic retinopathy
- E10.36 – Type 1 diabetes mellitus with diabetic cataract
- E10.37 – Type 1 diabetes mellitus with diabetic macular edema
- E10.39 – Type 1 diabetes mellitus with other diabetic ophthalmic complication
These codes specify the type of diabetes (type 1 or type 2) and the severity or specific complication of diabetic retinopathy. The ICD-10 coding system is used for medical billing, statistical purposes, and clinical documentation. Proper coding helps healthcare providers and insurance companies identify and categorize specific conditions, facilitating appropriate care and reimbursement processes. If you have been diagnosed with diabetic retinopathy, your healthcare provider will assign the appropriate ICD-10 code in your medical records.
