Everything you need to know about glaucoma and glaucoma treatments
What is Glaucoma?
Glaucoma is a group of eye disorders that cause damage to the optic nerve, leading to vision loss or blindness if left untreated. It is often associated with elevated intraocular pressure (IOP), but it can also occur at normal or even low IOP levels. Glaucoma is a leading cause of irreversible blindness worldwide and affects millions of people, especially those over the age of 60. The condition develops gradually and is usually painless, which makes regular eye exams essential for early detection and treatment.
Types of Glaucoma:
1. Open-Angle Glaucoma:
This is the most common type of glaucoma, accounting for about 90% of cases. Our eyes are filled with fluid (aqueous humor) that nourishes the eye and helps maintain its shape. This fluid is continuously produced and drained from the eye. With open-angle glaucoma the fluid drainage becomes less efficient over time (like a clogged drain). As a result, eye pressure builds up and starts to damage the optic nerve. This type of glaucoma is painless and causes no vision changes at first. Some people have optic nerves that are sensitive to normal eye pressure. This means their risk of getting glaucoma is higher than normal. This type of glaucoma is called low-tension glaucoma.
Regular eye exams are important to find early signs of damage to their optic nerve.
2. Angle-Closure Glaucoma:
This type of glaucoma , also known as closed-angle or narrow-angle glaucoma, occurs when someone’s iris is very close to the drainage angle in the eye. The iris can end up blocking the drainage angle completely (like a piece of paper sliding over a sink drain). This will cause eye pressure to rise very quickly. This is called acute glaucoma. It is a true eye emergency as it can lead to rapid, permanent vision loss and intense eye pain. You should call your ophthalmologist right away or you might go blind permanently.
3. Normal-Tension Glaucoma:
In this type, optic nerve damage and vision loss occur despite normal IOP levels.
The exact cause is not fully understood, but it is believed to be related to poor blood flow to the optic nerve.
4. Secondary Glaucoma:
This type of glaucoma is a result of another eye condition or an underlying medical condition or medication that affects the drainage of eye fluid.

Causes and Risk Factors:
The exact cause of most glaucoma cases remains unknown, but several risk factors contribute to its development, including:
- The risk of glaucoma increases with age, especially after 60.
- If you have a family history of glaucoma, your risk of developing the condition is higher.
- Increased pressure within the eye is a significant risk factor for optic nerve damage and glaucoma.
- People of African, Asian, and Hispanic descent are at higher risk for certain types of glaucoma.
- Individuals with thinner corneas may be at increased risk.
- Diabetes, high blood pressure, and heart disease may increase the risk of glaucoma.
- Previous eye trauma or surgery can increase the risk of glaucoma.
Glaucoma Symptoms
In the early stages, glaucoma does not cause noticeable symptoms. As the condition progresses, individuals may experience:
- Glaucoma typically affects peripheral vision first, causing a gradual reduction in the ability to see objects or movement to the side. This loss may go unnoticed for a long time because central vision remains clear.
- As the disease progresses, the field of vision may continue to narrow, leading to tunnel vision. This means only a small, central area of sight remains, while the rest of the visual field is lost.
- Individuals with glaucoma may experience blurred or hazy vision, especially in the early stages of the condition.
- Glaucoma can cause halos or rainbow-colored rings to appear around lights, making it challenging to see clearly, particularly in low-light conditions.
- In some cases of acute angle-closure glaucoma, sudden and severe eye pain, along with headaches, may occur, accompanied by nausea and vomiting.
- Glaucoma can lead to redness in the affected eye, particularly during episodes of increased eye pressure.
It is essential to note that vision loss from glaucoma is irreversible, and any lost vision cannot be restored. Early detection and timely treatment are crucial to slow or halt the progression of the disease and preserve remaining vision.

Glaucoma Diagnosis
The diagnosis of glaucoma involves a comprehensive eye examination conducted by an ophthalmologist.. As glaucoma can develop without noticeable symptoms in the early stages, regular eye exams are crucial, especially for individuals at higher risk due to age, family history, or other factors. The diagnosis typically includes the following steps:
1. Patient History: The eye care professional will start by gathering information about the patient’s medical history, including any family history of glaucoma or other eye conditions.
2. Visual Acuity Test: This test measures how well the patient can see at various distances using an eye chart.
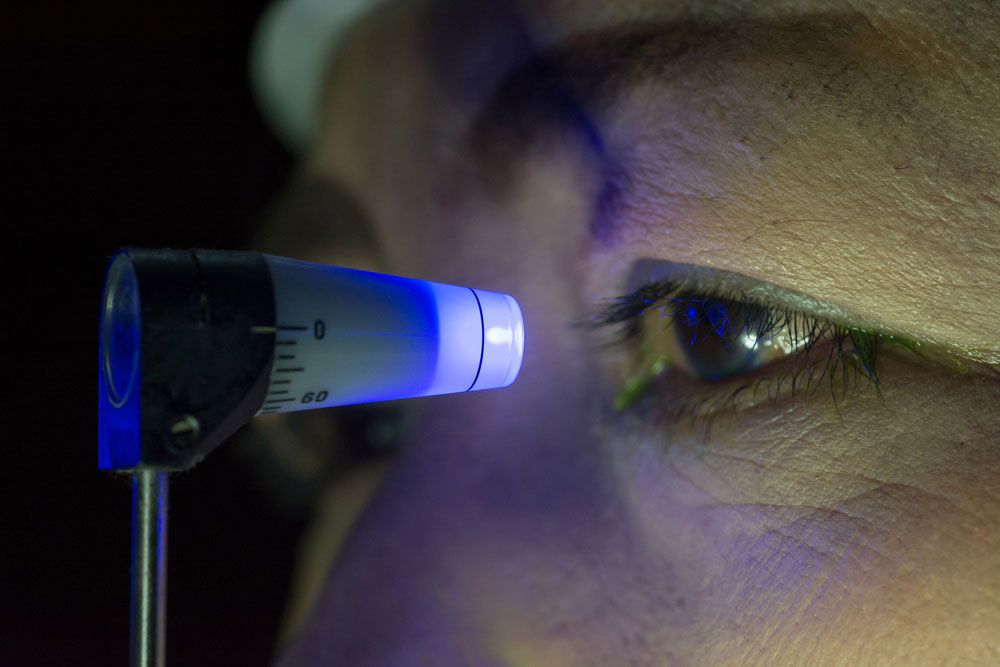
3. Tonometry: Tonometry is used to measure intraocular pressure (IOP), which is a key risk factor for glaucoma. There are different types of tonometry, including:
- Goldmann Applanation Tonometry: The patient’s eye is numbed with eye drops, and a device gently touches the cornea to measure IOP.
- Non-Contact Tonometry: A puff of air is used to estimate IOP without touching the eye.
4. Pachymetry: This test measures the thickness of the cornea, as corneal thickness can influence IOP readings.
5. Gonioscopy: Gonioscopy is used to assess the drainage angle of the eye. A special contact lens with a mirror is placed on the eye, allowing the eye care professional to see the drainage angle’s structure.
6. Optic Nerve Assessment: The ophthalmologist will use an ophthalmoscope or a specialized lens to examine the optic nerve and look for any signs of damage, such as thinning of the nerve fibers or changes in the cup-to-disc ratio. In order to visualize the optic nerve and the retina as good as possible, dilating drops will be used to enlarge the pupils.
7. Visual Field Testing: Also known as perimetry, this test assesses the patient’s peripheral vision. It helps detect any characteristic patterns of vision loss associated with glaucoma.
8. Imaging: Optical coherence tomography (OCT) is used to obtain detailed images of the optic nerve and assess its health.
9. Regular Follow-Up: If glaucoma is suspected or diagnosed, the patient will be scheduled for regular follow-up appointments to monitor the condition’s progression and response to treatment.
Glaucoma treatments
To manage glaucoma effectively, a variety of treatments are available, each tailored to the patient’s specific needs and the type and severity of the condition. The various glaucoma treatments play a crucial role in preserving sight and enhancing the quality of life for those affected by this eye disorder.
Eye Drops
Eye drops are commonly prescribed as the first line of treatment for glaucoma. These medications work by either reducing the production of eye fluid (aqueous humor) or increasing its drainage to lower IOP. There are several classes of eye drops used in glaucoma management:
- Prostaglandin Analogs: These eye drops increase the drainage of aqueous humor, reducing IOP. They are usually administered once daily and have shown to be highly effective in controlling glaucoma progression.
- Beta-Blockers: These eye drops decrease the production of aqueous humor, thereby reducing IOP. They are often prescribed as first-line treatment and can be used in combination with other eye drops.
- Alpha Agonists: These eye drops both reduce the production of aqueous humor and increase its drainage. They are often used as an adjunct to other eye drops.
- Carbonic Anhydrase Inhibitors: Available in both topical and oral forms, these eye drops decrease aqueous humor production and are used when other medications are ineffective.
Oral Medications
In some cases, oral medications may be prescribed in addition to or instead of eye drops to manage glaucoma. Carbonic anhydrase inhibitors are commonly used in oral form to reduce IOP.
Laser Treatment
- Laser Trabeculoplasty: This procedure is often employed for open-angle glaucoma. It uses a focused laser beam to treat the drainage angle of the eye’s trabecular meshwork, improving the outflow of aqueous humor and reducing IOP.
- Laser Peripheral Iridotomy (LPI): This laser procedure is beneficial for angle-closure glaucoma. It creates a small hole in the iris, allowing aqueous humor to flow more freely and alleviating elevated IOP.
Surgery
When eye drops and laser therapy are inadequate, surgical interventions become necessary to control IOP effectively. Some common surgical procedures include:
- Trabeculectomy: This is a traditional glaucoma surgery where a new drainage channel, called a bleb, is created to facilitate the outflow of aqueous humor and lower IOP.
- Glaucoma Drainage Devices (GDDs): These are implantable devices that provide a controlled pathway for aqueous humor to drain, helping to manage IOP in refractory glaucoma cases.
- Minimally Invasive Glaucoma Surgery (MIGS): MIGS procedures are relatively new and involve less invasive techniques to enhance the outflow of aqueous humor. These surgeries are often combined with cataract surgery for maximum effect.
Cyclophotocoagulation
Cyclophotocoagulation uses a laser to target and decrease the production of aqueous humor by treating the ciliary body. It is often considered in cases where other treatments have failed or are unsuitable.
The many glaucoma treatment options all have the same purpose: preventing optic nerve damage (and permanent vision loss) by decreasing the intraocular pressure.
The choice of treatment depends on various factors, including the type and severity of glaucoma, the patient’s overall health, and their individual preferences. Regular follow-up visits with an ophthalmologist or glaucoma specialist are crucial to monitor the condition’s progression, assess the effectiveness of the treatment, and make any necessary adjustments. Early detection, prompt intervention, and consistent management are vital in preserving vision and maintaining a good quality of life for those living with glaucoma. If you suspect you have glaucoma or have been diagnosed with the condition, consult your eye care professional for personalized advice and treatment.
