The retina, a thin and sensitive layer of nerve tissue at the back of the eye, plays a pivotal role in the process of vision. It functions as a sophisticated light sensor, receiving images from the outside world and converting them into electrical signals, which are then transmitted to the brain via the optic nerve. Any damage to the retina, no matter how small, can severely impact vision, potentially leading to permanent blindness. Therefore, early recognition of symptoms and proactive prevention of retinal diseases are crucial for protecting your sight and maintaining a high quality of life.
This article is a detailed, in-depth guide to common retinal conditions, covering their causes, disease mechanisms, signs, and the most advanced diagnostic and treatment methods available today. More importantly, we will provide practical and actionable advice on how to prevent retinal diseases so you can scientifically and effectively protect your “windows to the soul,” especially given the increasing prevalence of high-risk systemic diseases.
Detailed Anatomy and Function of the Retina
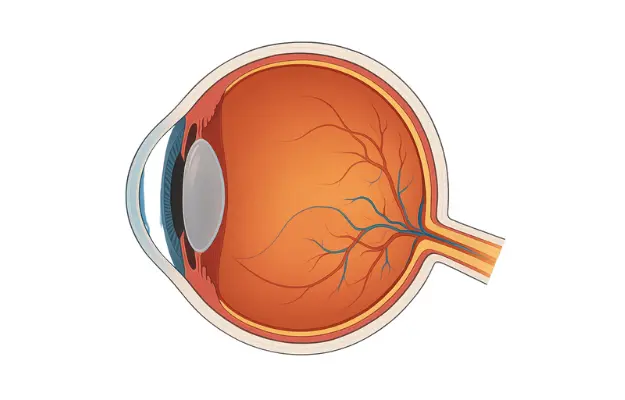
To gain a deeper understanding of retinal diseases, we first need to grasp the complex structure and remarkable function of this tissue. The retina is not a simple layer but a multi-layered structure composed of several specialized cell types:
- Photoreceptor Cells: This is the first layer of cells to receive light. It consists of two main types:
- Rods: Responsible for peripheral vision and the ability to see in low-light conditions (night vision). They are highly sensitive to light but do not perceive color.
- Cones: Primarily concentrated in the macula, they are responsible for sharp, detailed central vision and color perception.
- Macula: A small, central area of the retina densely packed with cone cells. The macula is the “hot spot” of the retina, responsible for all visual activities that require high acuity, such as reading, driving, and recognizing faces.
- Retinal Blood Vessels: A dense network of arteries and veins that supply the retina with oxygen and nutrients. Any damage to this network is the primary cause of many serious retinal diseases.
The synchronized activity of these cells and blood vessels gives us clear and complete vision. When any part is damaged, the entire system is affected.
Common Retinal Diseases: Causes, Signs, and Diagnosis
Retinal diseases are diverse but can be better understood and categorized by their underlying mechanisms.
Diabetic Retinopathy
This is one of the most severe and common complications of diabetes, and it’s the leading cause of blindness in working-age adults. The disease progresses silently and is divided into several stages.
Disease Mechanism
High blood sugar levels over an extended period damage the walls of the retinal blood vessels, making them weak, prone to leakage, or blockage.
- Non-proliferative Diabetic Retinopathy (NPDR): In this early stage, small blood vessels swell, leak fluid and lipids, causing retinal and macular edema, and leading to vision loss. This stage often has no clear symptoms.
- Proliferative Diabetic Retinopathy (PDR): To compensate for blocked blood vessels, the body grows new, abnormal blood vessels (neovascularization). These new vessels are very fragile and can rupture easily, causing vitreous hemorrhage, forming scar tissue, and potentially leading to tractional retinal detachment.
Signs and Symptoms
- Early stage: Often asymptomatic. This is why regular eye exams are mandatory for people with diabetes.
- Advanced stage: Patients may suddenly notice dark spots or floating strands (floaters) in their vision due to hemorrhage.
- Blurred vision or a sudden decrease in visual acuity.
- Complete vision loss if the retina detaches or a severe hemorrhage occurs.
Diagnosis
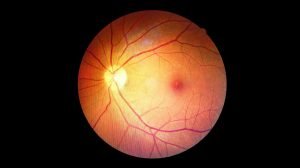
A doctor performs a dilated fundus examination. Advanced imaging techniques like Optical Coherence Tomography (OCT) are used to assess the extent of macular edema, while Fluorescein Angiography (FFA) helps identify the location and degree of blood vessel leakage.
High-Risk Individuals
People with type 1 and type 2 diabetes, especially those who have had the disease for many years and have poor control over their blood sugar, blood pressure, and cholesterol.
>> Preventing Diabetic Retinopathy: Comprehensive Vision Protection for Diabetics
Age-Related Macular Degeneration (AMD)
AMD is the leading cause of central vision loss in older adults, directly affecting the ability to read, drive, and recognize faces.
Disease Mechanism
Aging causes damage to the photoreceptor cells and supporting tissue layers in the macula. Based on the mechanism of damage, AMD is divided into two forms:
- Dry AMD: Accounts for 85-90% of cases. It’s caused by the accumulation of cellular waste products (drusen) and the gradual degeneration of photoreceptor cells. This form progresses slowly but can transition to the wet form.
- Wet AMD: Accounts for 10-15% of cases but is more severe. It’s caused by the growth of abnormal blood vessels from the choroid underneath the retina. These vessels leak fluid and blood, causing swelling, scarring, and permanent damage to the macula in a short period.
Signs and Symptoms
- Blurred, distorted central vision. Straight lines may appear curved or wavy.
- Difficulty seeing details when reading or doing fine-motor tasks.
- A blind spot appears in the center of vision.
Diagnosis
Doctors use tools like the Amsler grid to check central vision, a fundus examination, OCT to assess macular structure, and FFA to detect abnormal blood vessels.
High-Risk Individuals
People over 60, those with a family history of AMD, smokers, and individuals with a poor diet lacking antioxidants.
>> Age-Related Macular Degeneration (AMD): Causes, Symptoms, and Prevention
Retinal Detachment
Retinal detachment is an ophthalmic emergency where the retina separates from its underlying nourishing tissue, causing severe and potentially permanent vision loss if not treated promptly.
Disease Mechanism
- Rhegmatogenous Detachment (most common): The vitreous humor inside the eye shrinks with age, pulling on the retina and causing a tear. Fluid seeps through the tear and accumulates under the retina, causing it to detach.
- Tractional Detachment: Often seen in people with proliferative diabetic retinopathy. Scar tissue from the abnormal new vessels pulls the retina away from its position.
- Exudative Detachment: Fluid leaks from abnormal blood vessels (due to inflammation or tumors) and accumulates under the retina without a tear.
Signs and Symptoms
- Sudden flashes of light (photopsia), especially in one eye and when the head moves.
- A sudden increase in dark spots or “floaters.”
- A shadow or curtain appearing from the periphery and moving towards the center of vision.
Diagnosis
A doctor will examine the retina with a fundus examination and ultrasound to determine the location and extent of the detachment.
High-Risk Individuals
People with severe myopia, a history of eye trauma, previous eye surgery, or diabetic retinopathy.
>> Retinal Detachment Surgery: Causes, Procedure, and Effective Treatment Methods
Effective and Scientific Retinal Disease Prevention
Prevention is always better than cure, especially with retinal diseases, which can leave permanent damage if not caught and treated in time.
Regular and Specialized Eye Exams
This is the single most important preventative measure. A routine eye exam should include more than just a refraction check; it should involve a specialized retinal examination. An ophthalmologist will use advanced equipment to perform a dilated fundus exam, Optical Coherence Tomography (OCT), or Fluorescein Angiography (FFA) to detect early signs of retinal damage, even before you experience any symptoms.
Exam Frequency:
- General Population: A comprehensive eye exam every 1-2 years.
- High-Risk Individuals: A specialized retinal exam every 6-12 months, or as directed by a doctor.
- People with Diabetes: Must have an eye exam at least once a year, even if their vision seems fine.
Strict Control of Systemic Diseases
Many retinal diseases are complications of other systemic conditions, so managing these diseases is the best way to protect your retina.
- Diabetes: Maintaining stable blood sugar levels (HbA1c < 7%), blood pressure, and cholesterol within a healthy range is the most effective way to prevent and slow the progression of diabetic retinopathy.
- Hypertension: High blood pressure can also damage retinal blood vessels, leading to hypertensive retinopathy and increasing the risk of retinal vascular occlusion.
- Cardiovascular Disease: Heart disease can also affect blood flow to the eyes, raising the risk of retinal artery or vein occlusion.
A Scientific and Nutritious Diet
A diet rich in key nutrients and antioxidants can protect the retina from damage caused by free radicals.
- Lutein and Zeaxanthin: These are powerful carotenoids concentrated in the macula that help filter blue light and protect retinal cells. They are abundant in dark leafy greens (kale, spinach), corn, and eggs.
- Vitamins C and E: As antioxidants, they help protect cells from damage. Found in oranges, strawberries, broccoli, and nuts.
- Zinc: Helps the retina maintain its health. Found in red meat, seafood, and beans.
- Omega-3 Fatty Acids: Help protect the retina and have anti-inflammatory properties. Found in fatty fish like salmon, herring, and walnuts.
Protecting Your Eyes from Environmental and Lifestyle Factors
- Wear Quality Sunglasses: When outdoors, wear sunglasses that block 100% of UVA and UVB rays to protect the retina from UV damage. UV exposure is a risk factor for macular degeneration and cataracts.
- Quit Smoking: Smoking doubles the risk of developing macular degeneration and increases the risk of many other eye diseases.
- Use Protective Eyewear: When playing sports or working in hazardous environments (welding, carpentry), wearing protective eyewear is the only way to prevent eye trauma.
- Limit Screen Time: Follow the 20-20-20 rule to reduce eye strain and fatigue.
Healthy Lifestyle Habits
- Regular Exercise: Improves blood circulation, helps control systemic diseases, and maintains overall eye health.
- Manage Weight: Obesity increases the risk of many diseases, including diabetes and hypertension, which indirectly affect the retina.
- Get Enough Sleep: Getting 7-8 hours of sleep each night allows the eyes to rest and recover.
>> Read more: Modern Eye Examination and Diagnostic Methods
Advanced Treatment Options
Once a retinal disease is diagnosed, timely treatment is crucial to preserve vision.
- Laser Photocoagulation: A laser is used to seal off abnormal blood vessels, preventing them from leaking or bleeding.
- Intraocular Injections: Anti-VEGF medications are injected into the eye to reduce swelling and stop the growth of abnormal blood vessels.
- Vitrectomy Surgery: An intraocular surgery to address complex issues like vitreous hemorrhage, tractional retinal detachment, or epiretinal membranes.
- Cryopexy (Cryotherapy): A freezing probe is applied to the outside of the eye to induce an inflammatory reaction that helps the retina reattach to the underlying tissue.
Conclusion
The retina is an indispensable component of vision. Retinal diseases can have severe consequences, but they are often preventable and treatable with early detection. By proactively caring for your eyes, maintaining a healthy lifestyle, and undergoing regular eye exams, you can protect your retina, preserve your vision, and enjoy life to the fullest.