Vision is one of our most precious senses, playing a pivotal role in our daily lives. However, over time, many people face eye problems, among which cataracts are one of the most common causes of vision loss, especially in older adults. So, what exactly are cataracts, what are their symptoms, and what are the effective treatment methods? This article provides a comprehensive overview of this condition, helping you understand more to protect your eyesight.
What Are Cataracts?
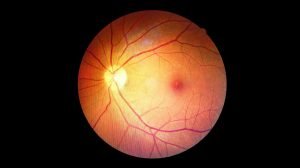
To understand cataracts, we first need to know about the eye’s natural lens. The natural lens of the eye is a crucial, transparent, biconvex structure located behind the iris and pupil. Its primary function is to focus light entering the eye onto the retina, allowing us to see objects clearly at various distances.
Cataract is a condition where the eye’s natural lens becomes cloudy or opaque, losing its transparency. When the lens becomes cloudy, light cannot pass through clearly to the retina, leading to blurred vision, cloudiness, or seeing everything as if through a misty veil. This condition can affect one or both eyes and typically develops gradually over time.
Essentially, a cataract is a natural aging process of the proteins within the lens. These proteins are initially arranged in an orderly fashion to keep the lens clear. However, with age or other factors, they can begin to clump together, forming cloudy areas that obstruct the passage of light. This is why cataracts are often considered a part of the eye’s natural aging process.

Causes of Cataracts
While age and aging are the primary causes, cataracts don’t only affect the elderly. Several other factors can contribute to their development:
- Age (Aging): This is the most common cause. After the age of 40, the risk of developing cataracts begins to increase significantly, and most people show some signs of cataracts by their 60s or 70s.
- Eye Injury/Trauma: A severe injury to the eye can damage the lens and cause a traumatic cataract.
- Underlying Medical Conditions: Certain chronic diseases can increase the risk of cataracts:
- Diabetes: Uncontrolled high blood sugar can alter the structure of the lens.
- Glaucoma: This condition can increase cataract risk, especially if long-term steroid eye drops are used.
- Medication Use: Long-term use of certain medications, particularly corticosteroids (oral or eye drops), can cause secondary cataracts.
- UV Radiation Exposure: Prolonged exposure of the eyes to sunlight without proper protection (UV-blocking sunglasses) can accelerate cataract formation.
- Smoking and Excessive Alcohol Consumption: Studies show that smoking and heavy alcohol consumption can increase the risk.
- Genetics: In some cases, cataracts can have a hereditary component or be present from birth (congenital cataracts).
- Previous Eye Surgery: Occasionally, other eye surgeries (e.g., glaucoma surgery) can lead to cataract development later.
- Radiation: Exposure to ionizing radiation (e.g., radiation therapy to the head and neck) can cause cataracts.
Understanding these risk factors helps us take preventive measures or seek early detection for timely intervention.
Signs and Symptoms of Cataracts
Cataracts typically develop slowly, and symptoms may not be obvious in the early stages. However, as the condition progresses, the signs become more pronounced, affecting the patient’s daily life.
Common Early Symptoms
- Blurred or Cloudy Vision: This is the most common symptom. Your vision may gradually become hazy, as if you’re looking through a dirty or misty window. The degree of blurriness can vary depending on the size and location of the cloudy area on the lens.
- Difficulty Seeing in Dim Light or at Night: Cataracts reduce the amount of light entering the eye. This makes it harder to see clearly in low-light conditions or when driving at night. Patients may notice glare or halos around lights when driving at night, causing uncomfortable brightness.
- Sensitivity to Bright Light (Glare): Light from the sun, car headlights, or bright indoor lights can become more uncomfortable and dazzling than usual.
- Fading or Yellowing of Colors: A cloudy lens can make the colors you see appear faded, less vibrant, or have a yellowish tint.
- Double Vision (Diplopia) in One Eye: In some rare cases, cataracts can cause double vision when looking with only one eye.
- Frequent Changes in Eyeglass Prescription: Initially, cataracts might alter the eye’s refractive error, causing you to need frequent changes in your eyeglass prescription. However, this is temporary and doesn’t address the root cause.
Impact on Daily Vision
As cataracts progress, daily activities requiring clear vision, such as reading, watching TV, using a computer, recognizing faces, or driving, become increasingly difficult. The quality of life can be significantly impacted. Patients may feel less confident, avoid social activities, and gradually become more dependent on others.
When to Consult an Eye Doctor?
If you start to notice any of the symptoms mentioned above, especially if they are significantly affecting your daily life or your ability to perform basic activities like driving or reading, you should see an eye doctor immediately. Regular eye exams, particularly for individuals over 40 and those with risk factors, are crucial for early detection and timely intervention. Your doctor will use a slit lamp to examine and accurately diagnose the cataract, while also performing a comprehensive eye and retina check.
Current Cataract Surgery Methods
Currently, surgery is the only and most effective method to treat cataracts. During the surgical procedure, the cloudy lens is removed and replaced with a clear artificial intraocular lens (IOL). This is one of the most common and safest surgeries worldwide.
Phacoemulsification (Phaco) Surgery
Phacoemulsification (Phaco) is the most advanced and widely used cataract surgery method today.
Principle:
The surgeon makes a tiny incision (about 2-3 mm) at the edge of the cornea. A small ultrasonic probe is inserted through this incision. High-frequency ultrasonic waves emulsify (break up) the cloudy lens into tiny fragments. These fragments are then suctioned out.
Artificial Intraocular Lens (IOL) Implantation:
After the cloudy natural lens is completely removed, a foldable artificial intraocular lens (IOL) is inserted and unfolded, settling into the position of the old lens. The posterior capsule of the lens is preserved to support the artificial lens. This procedure, known as Phacoemulsification, is the primary method for removing cataracts today.
Advantages:
- Very small incision, usually self-sealing and requires no stitches.
- Short surgery time (typically 30 minutes to 1 hour).
- Minimized complications and infection risk.
- Fast recovery time, patients can usually go home the same day.
- Vision results are typically excellent.
Femtosecond Laser-Assisted Cataract Surgery (FLACS)
FLACS is a newer technology that uses a Femtosecond laser to perform some surgical steps that were previously done manually.
Principle:
The Femtosecond laser is used to:
- Create precise incisions in the cornea.
- Create a perfectly circular opening in the anterior lens capsule (capsulorhexis), which aids in more accurate IOL removal and placement.
- Soften and fragment the cloudy lens, making the Phacoemulsification process quicker and requiring less ultrasonic energy.
Advantages:
- Increased precision and predictability of surgical outcomes.
- Reduced ultrasonic energy required, which can be beneficial for denser cataracts.
- Improved safety in some specific cases.
Disadvantages:
- Higher cost compared to traditional Phaco.
- Not all cases require or are suitable for laser-assisted surgery.
Comparison of Advantages and Disadvantages of Each Method
Criterion | Phacoemulsification (Phaco) Surgery | Femtosecond Laser-Assisted Cataract Surgery (FLACS) |
Technology | Ultrasonic waves to emulsify and remove the lens. | Femtosecond laser assists initial steps, then combined with Phaco. |
Incision | Micro-incision (2-3mm), created manually or with a diamond blade. | Micro-incision, precisely created by laser. |
Precision | Very high, depends on the surgeon’s experience. | Higher, automates some steps, less dependent on human factors. |
Ultrasonic Energy | Varies with lens density, can be higher. | Usually lower as the laser softens the lens first. |
Surgery Duration | Short (30-60 minutes). | Similar or slightly longer due to laser setup. |
Recovery Time | Fast, typically within a few days. | Similar, may be slightly faster for some individuals. |
Cost | More affordable. | Higher. |
Application | Common, suitable for most cataract cases. | Suitable for more complex cases, or patients desiring maximum precision. |
The choice of surgical method depends on the patient’s specific eye condition, the density of the cataract, overall health, and the eye surgeon’s recommendation.
>> Modern Treatments and Surgical Methods for Eye Conditions
Types of Artificial Intraocular Lenses (IOLs) Used in Surgery
A crucial factor determining vision results after cataract surgery is the type of artificial intraocular lens (IOL) implanted. There are various types of IOLs, each with its own advantages:
- Monofocal IOLs: These are the most basic type of IOL, providing a single focal point, usually for distance vision. After surgery, patients typically still need to wear glasses for near vision (reading, using a phone) or intermediate vision.
- Multifocal IOLs: These IOLs allow patients to see clearly at multiple distances (distance, intermediate, near), reducing dependence on glasses after surgery. However, some patients may experience halos or glare at night.
- Accommodative IOLs: These IOLs are designed to move or change shape within the eye, mimicking the natural accommodation ability of the lens, allowing for clear vision at various distances.
- Toric IOLs: Designed for patients with astigmatism. Toric IOLs help correct astigmatism during cataract surgery, reducing or eliminating the need for astigmatism-correcting glasses afterward.
For patients experiencing both cataracts and presbyopia (age-related farsightedness), the PRELEX (Presbyopia-Correcting Lens Exchange) procedure is an ideal option, replacing the old lens with a multifocal IOL, improving vision at multiple distances and eliminating the need for reading glasses. Your eye doctor will recommend the most suitable IOL based on your visual needs, lifestyle, and eye condition.
The Cataract Surgery Process
To ensure a safe and effective surgical outcome, patients must strictly follow pre-, intra-, and post-operative instructions.
Before Surgery
- Comprehensive Eye Examination: Patients will need a thorough eye exam to comprehensively assess their eye health. This includes checking the retinal condition, measuring the cataract’s density, and crucially, measuring the eye’s dimensions (biometry) to calculate and select the most suitable artificial intraocular lens with the correct refractive power. If the retina has issues (e.g., macular degeneration, diabetic retinopathy), the doctor will usually advise appropriate retinal treatment before proceeding with cataract surgery.
- Discussion with the Doctor: Patients will have the opportunity to discuss different IOL types and decide which is best suited for their visual needs.
- Stopping Certain Medications: The doctor may request that you stop using certain blood-thinning medications or others before surgery to reduce the risk of bleeding.
- Mental Preparation: Cataract surgery is a safe procedure; patients should maintain a relaxed mindset and trust their doctor.
During Surgery
Cataract surgery is an outpatient procedure, typically lasting 30 minutes to 1 hour, allowing patients to recover at home.
Anesthesia:
Before surgery, nurses will use special eye drops to dilate the pupil and numb the eye. The surgeon may also use light sedation to help you feel more comfortable and relaxed if needed. Patients will be awake throughout the procedure but will not feel pain.
Procedure:
- The surgeon makes a tiny incision (2-3mm) in the cornea.
- Ultrasonic waves (Phaco method) or a laser (FLACS method) are used to emulsify and remove the cloudy lens.
- After the cloudy lens is completely removed, a foldable artificial intraocular lens is implanted inside the eye, settling into the position of the natural lens.
Completion:
The micro-incision usually self-seals without stitches. The eye will be covered with a patch or protective shield.
After Surgery and Recovery
- Immediately After Surgery: Your eye will be patched and removed the next day at your post-operative consultation. Initially, your vision may still be slightly blurry or feel mildly uncomfortable, which is completely normal.
- First Few Days: Other issues like itching and discomfort may appear in the days following, so you must strictly avoid rubbing your eyes during this period. Your eye doctor may instruct you to wear protective eyewear (often during sleep or outdoors) and use prescribed eye drops (antibiotics and anti-inflammatories) exactly as scheduled to prevent infection and reduce swelling.
- Vision Improvement: After the eye patch is removed, your vision should improve significantly. Sometimes, you may need a few more days for your vision to fully stabilize due to post-operative swelling.
- Follow-up Appointments: Patients need to adhere to scheduled follow-up appointments with the doctor to ensure the eye is recovering well and there are no complications.
- Daily Activities: The doctor will provide specific instructions on activities to avoid during the recovery phase, such as avoiding heavy lifting, excessive bending, swimming, or exposure to dust for a certain period.
Most patients achieve excellent vision after cataract surgery. Some may still need to wear mild corrective glasses for distance or near vision depending on the type of IOL implanted.
Post-Operative Eye Care and Expert Advice
Proper eye care after surgery is key to ensuring the best possible outcome and preventing complications.
- Use Eye Drops Correctly: This is extremely important. Follow the dosage and schedule prescribed by your doctor.
- Avoid Rubbing or Pressing the Eye: The eye after surgery is very delicate and easily damaged.
- Wear Protective Eyewear: Use protective glasses or an eye shield (often during sleep) to guard against accidental impact.
- Avoid Contaminated Water and Chemicals: Do not swim, use saunas, or let soap or shampoo get into your eye for the first few weeks.
- Limit Strenuous Activities: Avoid heavy lifting, strenuous exercise, or activities that could increase pressure on the eye.
- Protect Eyes from Sunlight: Wear sunglasses outdoors to protect your eyes from UV rays and reduce glare.
- Attend Follow-up Appointments: Do not miss any scheduled follow-up appointments with your doctor to check on your eye’s recovery progress.
- Nutrition and Lifestyle: Maintain a healthy diet rich in vitamins A, C, E, and antioxidants. Limit smoking and alcohol consumption.
>> Read more: Effective Treatment of Blepharitis with BlephEx
Frequently Asked Questions About Cataracts (FAQ)
Q1: Can cataracts be cured with eye drops or oral medication?
A1: No. Currently, there are no eye drops, oral medications, or non-surgical treatments that can cure or slow the progression of cataracts. Surgery is the only way to remove the cloudy lens and restore vision.
Q2: Is cataract surgery painful?
A2: No. Surgery is typically performed under local anesthesia, possibly combined with mild sedation. Patients will be awake but will not feel pain during the procedure. After surgery, there might be mild discomfort or itching, but this can usually be managed with over-the-counter pain relievers.
Q3: Do I need to have both eyes operated on at the same time?
A3: Usually not. Cataract surgery is typically performed on one eye at a time, with a recovery period between surgeries (often several weeks) to allow the first eye to heal completely and to assess the outcome. This also minimizes the risk of complications if an issue occurs with one eye.
Q4: Can my vision get worse after surgery?
A4: Serious complications after cataract surgery are very rare. However, like any surgery, there is always a small risk of complications such as infection, bleeding, swelling, or retinal detachment. Most complications are treatable. The success rate of cataract surgery is very high (over 95%).
Q5: Are “cataracts” and “glaucoma” the same thing?
A5: No. “Cataract” refers to the clouding of the eye’s natural lens. “Glaucoma” is a different eye condition that causes damage to the optic nerve due to increased pressure inside the eye, which can lead to permanent vision loss. These two conditions are entirely different and require separate treatment methods.
Q6: Can the artificial lens get cloudy again after surgery?
A6: The artificial intraocular lens itself will not become cloudy. However, some patients may experience a condition called “posterior capsular opacification” (PCO), where the posterior capsule (the part retained to hold the IOL) becomes cloudy. This condition can be easily and quickly treated with a non-invasive laser procedure called YAG Laser Capsulotomy.
Q7: When should I consider cataract surgery?
A7: The decision for surgery is usually made when cataracts significantly begin to affect your daily quality of life, making it difficult to perform activities like reading, driving, or working. Your eye doctor will assess the degree of vision impairment and advise on the most suitable time for surgery.
Conclusion
Cataracts are a common condition, especially with increasing age. While they can cause significant vision loss, with the advancements in modern medicine, cataract surgery has become a safe and highly effective procedure, helping millions of people regain clear vision. Early recognition of symptoms, regular eye exams, and adherence to your doctor’s instructions are key to maintaining healthy eyes and preserving your quality of life. If you have any questions about cataract surgery or other eye care services, do not hesitate to contact the experts at European Eye Center for detailed consultation and answers.