Ocular albinism is a fairly rare congenital condition where the eyes, and sometimes the skin and hair, lack melanin pigment. Melanin is incredibly important; it doesn’t just provide color, but also protects the eyes and is vital for normal vision development. When there isn’t enough melanin, the eyes become more sensitive to light, and the ability to see is also affected.
So, what is ocular albinism, what causes it, and how can we manage this condition effectively? This article will help you understand everything you need to know about eye pigment disorders so that those affected can live the fullest lives possible.
What is Ocular Albinism? Why is Pigment So Important?
Ocular albinism is a group of rare, inherited conditions characterized by a reduction or complete absence of melanin pigment in eye structures like the iris (the colored part of the eye), retina, and choroid. Sometimes, this condition also affects the skin and hair, making them very light in color.
Did you know, melanin doesn’t just give your eyes their color; it plays a crucial role:
- Eye Protection: Melanin acts like a natural “sunglass” protecting your eyes from harmful ultraviolet (UV) rays from the sun.
- Vision Development: This pigment is essential for the proper development of the retina, especially the fovea (the central part of the retina that helps us see fine details).
When there’s not enough melanin, the eyes become:
- Extremely sensitive to light (easily bothered by bright light, also called photophobia).
- Vision is reduced because the fovea doesn’t develop fully.
- Lighter in color, and sometimes the iris can be translucent, revealing the red blood vessels in the retina, making the eyes appear pink or reddish in some cases.
>> Common Retinal Diseases and Effective Prevention Methods
Causes and Common Types of Ocular Albinism
Ocular albinism is primarily caused by genetic mutations inherited from parents. Depending on which gene is affected and the degree of melanin deficiency, the condition can manifest in different ways.
Ocular Albinism (OA)
This is the type where pigment deficiency is primarily or almost exclusively limited to the eyes. The skin and hair color of affected individuals are usually normal or only slightly lighter than other family members.
Causes: The most common form of OA is X-linked ocular albinism, caused by a mutation in the GPR143 gene (also known as OA1). This form predominantly affects males, while females are usually carriers and show fewer severe symptoms.
Oculocutaneous Albinism (OCA)
This is a more common type, characterized by pigment deficiency not only in the eyes but also noticeably in the skin and hair. There are several types of OCA, with OCA1 and OCA2 being the most common.
- OCA1: Caused by a mutation in the TYR gene, which is responsible for producing the enzyme tyrosinase—essential for melanin synthesis.
- OCA1A: Complete absence of tyrosinase, resulting in pure white skin and hair, and reddish eyes.
- OCA1B: Some tyrosinase activity, meaning skin and hair may develop a little pigment over time.
- OCA2: Caused by a mutation in the OCA2 gene, also involved in melanin production. Affected individuals typically have creamy white or light yellow skin, hair, and eye color.
Other Related Syndromes
Ocular albinism can also be part of more complex syndromes, affecting multiple organ systems beyond the eyes. For example:
- Hermansky-Pudlak Syndrome (HPS): Causes oculocutaneous albinism along with platelet dysfunction (leading to easy bleeding) and potential problems with the lungs or kidneys.
- Chédiak-Higashi Syndrome: Causes oculocutaneous albinism along with immune system deficiencies and neurological problems.
Understanding the genetic causes is extremely important for accurate diagnosis and for providing genetic counseling to families.
Recognizing the Signs of Ocular Albinism
The symptoms of ocular albinism primarily involve vision and the appearance of the eyes. The severity can vary depending on the type and degree of pigment deficiency.
Vision Problems:
- Reduced Vision: This is the most common and often the most significant symptom. Vision can range from mildly impaired to very poor, and it often cannot be fully corrected with standard eyeglasses. This is because of abnormal foveal development (foveal hypoplasia) and visual pathway abnormalities.
- Nystagmus: The eyes make involuntary, rapid, and repetitive movements. This is a very characteristic feature of ocular albinism and is often noticeable from early childhood. This condition can worsen with stress or fatigue.
- Photophobia (Light Sensitivity): Due to the lack of protective melanin, the eyes become extremely sensitive to bright light, causing discomfort and constant squinting.
- Strabismus (Crossed Eyes/Squint): The eyes are not properly aligned and may point in different directions.
- Reduced Stereopsis (Depth Perception): Difficulty perceiving depth, which can impair the ability to judge distances.
- Refractive Errors: Often accompanied by significant nearsightedness, farsightedness, or astigmatism.
External Eye and Body Characteristics:
- Pale Iris Color: The iris may be a very light blue, light gray, or even pink/red. This reddish appearance is due to light shining through the translucent, pigment-deficient iris, revealing the blood vessels in the retina.
- Pale Hair and Skin: In cases of oculocutaneous albinism (OCA), hair can be white or very light yellow, and the skin is very fair and prone to sunburn.
These signs are often detected early in infancy or childhood, sometimes immediately after birth.
How is Ocular Albinism Diagnosed?
Diagnosing ocular albinism usually involves a combination of clinical examination, specialized eye tests, and genetic testing.
Comprehensive Eye Exam:
- Vision Assessment: Evaluating the degree of vision impairment.
- Iris and Pupil Assessment: Observing iris color, pupil response to light, and how much light passes through the iris.
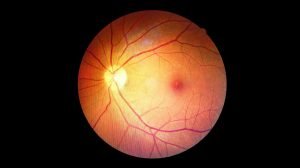
- Fundus Examination: Checking the retina for signs of foveal hypoplasia—a key diagnostic feature. The doctor will also look for pigment deficiency in the retina.
- Electroretinography (ERG): Assessing the function of light-sensitive cells in the retina.
- Optical Coherence Tomography (OCT): Provides detailed images of retinal structure, helping confirm foveal hypoplasia.
- Nystagmus Monitoring: Observing and recording involuntary eye movements.
- Visual Pathway Examination: Assessing for abnormal crossing (misrouting) of optic nerve fibers using specialized techniques.
Assessment of Systemic Features:
If oculocutaneous albinism is suspected, the doctor will examine skin and hair color, as well as signs of related syndromes.
Genetic Testing:
This is the most accurate method for confirming ocular albinism diagnosis. A blood or saliva sample will be taken for DNA analysis to look for relevant gene mutations. Genetic testing not only confirms the diagnosis but also helps with genetic counseling for families regarding recurrence risk in future pregnancies.
Treatment and Management of Ocular Albinism
Currently, there is no cure for ocular albinism because it’s an inherited condition. However, many measures aim to manage symptoms, optimize vision, and improve the quality of life for affected individuals.
Vision Improvement:
- Corrective Lenses (Glasses and Contact Lenses): Correcting refractive errors like nearsightedness, farsightedness, or astigmatism to achieve the best possible vision. Tinted contact lenses or special contact lenses can help reduce glare.
- Low Vision Aids: Using magnifiers, telescopes, or other magnifying devices to help individuals see better for reading, watching TV, or detailed tasks.
- Nystagmus Surgery: In some cases, surgery may be considered to reduce nystagmus, which can partially improve vision and head posture.
- Strabismus Surgery: Helps improve eye alignment and cosmetic appearance.
Eye Protection from Light:
- Sunglasses or Tinted Lenses: Wearing high-quality sunglasses with 100% UV protection is extremely important to protect the eyes from sun damage and significantly reduce light sensitivity. Lenses with amber, brown, or grey tints are often recommended.
- Wide-brimmed Hats, Umbrellas: Minimizing direct exposure to sunlight, especially during peak hours.
Educational and Vocational Support:
- Electronic Magnification Devices: E-readers, tablets with magnification functions, or magnification software on computers.
- Appropriate Lighting: Using indirect, sufficient, but not overly bright lighting.
- Favorable Seating Position: Sitting closer to whiteboards/screens at school or work.
- Special Educational Support: Collaborating with educators to ensure a learning environment that accommodates visual needs.
- Orientation and Mobility Training: Developing skills for safe navigation and movement in new environments.
Genetic Counseling and Psychological Support:
- Genetic Counseling: Crucial for families affected by ocular albinism to understand the genetic risks and family planning options.
- Psychological Support: Ocular albinism can impact an individual’s self-esteem and mental well-being. Participating in support groups or seeking psychological counseling can help individuals and their families cope better with the condition.
Managing ocular albinism is a long-term, comprehensive process requiring coordination among various medical specialists and support from family and the community.
Living with Ocular Albinism
Living with ocular albinism requires adaptation and active support from the surrounding environment. Despite vision limitations, many individuals with ocular albinism can achieve success in education and careers with appropriate support.
- Actively Seek Support: Don’t hesitate to contact organizations that support visually impaired individuals and low vision specialists for advice on assistive devices and independent living skills.
- Strict Eye Protection: Always wear sunglasses or tinted lenses when outdoors, even on cloudy days. This not only reduces glare but also protects the eyes from long-term UV damage.
- Environmental Adaptations: Adjust lighting indoors and in the workplace; use high-contrast materials (e.g., black text on a white background); and arrange living spaces for convenience, removing obstacles.
- Develop Other Skills: Focus on developing other senses and independent living skills to compensate for limited vision, promoting greater autonomy.
- Maintain a Positive Attitude: Participate in social activities and sports (with appropriate modifications) to enhance overall quality of life and well-being.
Frequently Asked Questions About Ocular Albinism (FAQ)
Q1: Is ocular albinism contagious?
A1: No, ocular albinism is a congenital genetic condition, not an infectious disease. It is absolutely not contagious and cannot spread from person to person.
Q2: Can this condition be fully cured?
A2: Currently, there is no complete cure for ocular albinism because it’s caused by genetic mutations. Treatments focus on managing symptoms and optimizing remaining vision.
Q3: Can someone with ocular albinism drive?
A3: In most cases, individuals with ocular albinism do not meet the legal vision standards required to drive. Vision is often very low, and nystagmus also makes safe driving difficult.
Q4: Does ocular albinism worsen over time?
A4: The pigment deficiency and foveal hypoplasia itself typically do not significantly worsen over time in adults. However, vision can fluctuate or be affected by other factors like normal eye aging. Nystagmus may decrease or change slightly in adulthood.
Q5: Will children of someone with ocular albinism inherit the condition?
A5: This depends on the specific type of ocular albinism and its inheritance pattern (e.g., autosomal recessive, X-linked). Genetic counseling is essential to assess the specific risk for each family.
Q6: Are there studies on gene therapy for ocular albinism?
A6: Yes, the field of gene therapy is making significant progress, and many studies are underway to find ways to treat inherited eye conditions, including some forms of ocular albinism. However, these are still in the research phase and are not yet widely applied in clinical practice.
Conclusion
Ocular albinism is a complex condition with various manifestations and degrees of severity. While it cannot be cured, with early diagnosis and appropriate vision management strategies, individuals with the condition can still lead full and meaningful lives. It’s crucial to have the support of family, community, and healthcare professionals to help affected individuals reach their maximum potential.
If you or a loved one shows signs of ocular albinism, don’t hesitate to seek out an ophthalmologist or reputable eye center for a comprehensive examination and expert consultation.