Retinal Detachment Surgery
Comprehensive surgery for retinal detachment is a specialized ophthalmic procedure that involves reattaching a detached retina to the underlying tissue to restore vision and prevent permanent vision loss. Retinal detachment occurs when the retina, the thin, light-sensitive layer at the back of the eye, detaches or separates from its normal position. There are many causes for retinal detachment. These include holes in the retina, diabetes and trauma to the eye.
The surgical approach for retinal detachment varies based on the type and extent of detachment, as well as the surgeon’s preference and expertise.
How dangerous is retinal detachment?
Retinal detachment is a serious eye condition that can cause permanent vision loss if not treated promptly. It occurs when the retina becomes separated from its normal position at the back of the eye. Prompt medical attention and appropriate treatment are essential to prevent severe vision impairment. If you experience any symptoms of retinal detachment, such as sudden floaters, flashes of light, a shadow or a curtain in your vision, seek immediate medical evaluation to protect your eyesight.
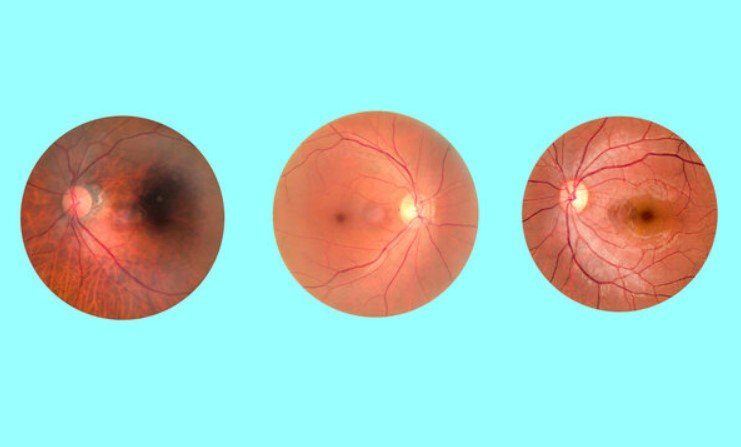
Retinal detachment diagnosis
- Initial Examination: The ophthalmologist will conduct a comprehensive eye examination, including visual acuity testing, pupil dilation, and examination of the retina using ophthalmoscopy or optical coherence tomography (OCT).
- Identifying the Type and Extent of Retinal Detachment: The surgeon will determine the type of retinal detachment (rhegmatogenous, tractional, or exudative) and assess its extent. This evaluation helps in planning the most appropriate surgical technique.
- Medical History and Imaging: The surgeon will review the patient’s medical history and may order additional imaging tests, such as ultrasound or fluorescein angiography, to further assess the retina’s condition.
Treatment: Surgical Techniques for Retinal Detachment
Vitrectomy:
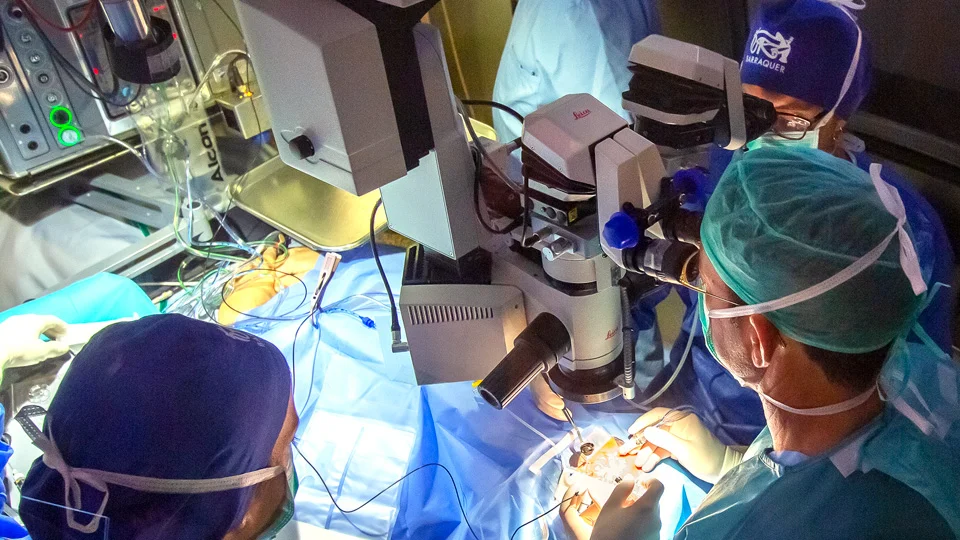
- During vitrectomy, the surgeon creates tiny incisions in the eye to gain access to the vitreous cavity (the space filled with a gel-like substance called vitreous).
- A vitrectomy probe is inserted to remove the vitreous gel, which allows better visualization and access to the retina.
- The surgeon uses microsurgical instruments, such as forceps, scissors, and laser probes, to repair any retinal tears or detachments.
- The surgeon may also use an endoillumination probe and a surgical microscope for enhanced visualization during the procedure.
Scleral Buckling:
- In cases where the retinal detachment is due to a retinal tear, the surgeon may use a scleral buckle. A scleral buckle is a silicone band or sponge that is placed on the outer surface of the eye (sclera).
- The buckle is secured around the eye and exerts inward pressure, indenting the sclera and helping the detached retina reattach to the underlying tissue.
Pneumatic Retinopexy:
- In pneumatic retinopexy, the surgeon injects a small, long-acting gas bubble into the vitreous cavity. The gas bubble floats upward and pushes the detached retina back against the eye wall.
- Once the retina is reattached, laser photocoagulation or cryotherapy is used to seal the retinal tear permanently.
- The patient’s head positioning is essential to ensure the gas bubble remains in contact with the detached retina during the healing process.
Combined Approaches:
- In some cases, the surgeon may use a combination of techniques, such as vitrectomy with scleral buckling or pneumatic retinopexy, depending on the complexity of the retinal detachment.
The Surgical Process
- Anesthesia: The surgery is typically performed under local or general anesthesia to ensure the patient’s comfort during the procedure.
- Creating Small Incisions: The surgeon creates small incisions in the eye to insert the surgical instruments and perform the necessary repairs.
- Vitrectomy (if applicable): In a vitrectomy, the surgeon removes the vitreous gel to gain access to the retina and address any retinal tears or detachments.
- Repairing Retinal Tears: Using microsurgical instruments and a surgical microscope, the surgeon identifies and repairs retinal tears with laser photocoagulation or cryotherapy. In some cases, additional procedures, such as the placement of retinal tamponade agents (e.g., gas or silicone oil), may be necessary.
- Scleral Buckling (if applicable): If a scleral buckle is used, the surgeon places the band or sponge around the eye and secures it in place to provide support to the detached retina.
- Pneumatic Retinopexy (if applicable): In pneumatic retinopexy, the surgeon injects a gas bubble into the eye, which gently pushes the detached retina against the eye wall. Laser or cryotherapy is then used to seal the retinal tear.
- Gas or Silicone Oil Injection (if applicable): In some cases, a gas bubble or silicone oil may be injected into the eye to provide support to the retina during healing. The choice between gas or oil depends on the surgeon’s judgment and the patient’s condition.
- Closing Incisions: The surgeon closes the small incisions in the eye with sutures or allows them to heal on their own, depending on the surgical technique used.

Post-operative Care
- Recovery Area: After surgery, the patient is usually monitored in a recovery area to ensure stability before discharge.
- Eye Patching: The eye may be patched for a short period to protect it during the initial healing phase.
- Medications: Prescription eye drops and/or oral medications are often prescribed to prevent infection, reduce inflammation, and manage pain.
- Activity Restrictions: Patients are advised to avoid strenuous activities and heavy lifting for several weeks to allow proper healing.
- Follow-up Visits: Regular follow-up appointments with the ophthalmologist are crucial to monitor the healing process, assess visual improvement, and address any potential complications.
- Gas Bubble Posturing (if applicable): In cases where a gas bubble is used, patients may be instructed to maintain a specific head position (posturing) to keep the bubble in contact with the detached retina for optimal reattachment.
- Vision Rehabilitation: Depending on the extent of retinal detachment and any resulting vision loss, patients may benefit from vision rehabilitation and low vision aids to maximize visual function.
Potential Risks and Complications
As with any surgical procedure, retinal detachment surgery carries some risks and potential complications, including:
- Infection
- Bleeding
- Increased intraocular pressure
- Cataract formation
- Recurrence of retinal detachment
- Vision loss or changes
- Double vision (diplopia)
- Complications related to anesthesia
Retinal detachment surgery is a complex and delicate procedure that requires the expertise of a skilled retinal surgeon. Most retinal detachment surgeries (80 to 90 percent) are successful if done on time, although a second operation is sometimes needed. Some retinal detachments cannot be fixed. The development of scar tissue is the usual reason that a retina can not be fixed. If the retina cannot be reattached, the eye will continue to lose sight and ultimately become blind.
The success of the surgery and the overall visual outcome depend on early diagnosis, appropriate surgical technique, and meticulous post-operative care. Patients should thoroughly discuss the procedure with their ophthalmologist, address any concerns, and closely follow the post-operative instructions to achieve the best possible results and preserve their vision effectively.
Retinal Detachment Surgery Cost in Vietnam
The cost of retinal detachment surgery can vary based on factors such as the severity of the detachment, the type of surgery required, the expertise of the surgeon, the specific medical facility, and any additional tests or post-operative care needed.
For accurate and up-to-date information about the cost of retinal detachment surgery in Vietnam, we recommend reaching out to reputable eye hospitals or clinics directly. They can provide you with specific details regarding the procedure’s cost, potential fees, and associated services.
When inquiring about the cost of retinal detachment surgery, it’s also important to ask about what the cost covers, including pre-operative assessments, surgical fees, anesthesia, hospital stays (if required), post-operative care, and follow-up appointments. Additionally, inquire about any potential financing options, insurance coverage, or available packages.
Please note that medical costs can change over time, so the most current information will be provided by the medical facilities themselves.
